Proton Therapy Case Study: Rare Pediatric Intracranial Myxoid Sarcoma
Presentation and Examination
A 12-year-old male presented with a one-month history of nausea and vomiting accompanied by progressive headaches radiating toward the frontal skull and behind the right eye
Diagnosis
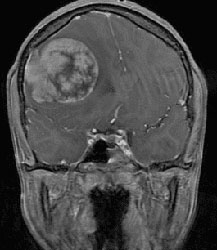
A brain MRI revealed a 5.7 x 5.5 x 5.0 cm large dural-based extra-axial enhancing mass in the right frontal region of the brain, with a dural tail that was invaginating into the right frontal lobe. As a result, edema and effacement of the right lateral and third ventricles had produced a 10 mm leftward shift—creating significant intracranial pressure.
A total spine MRI was negative for additional sites of disease.


Surgical Management
The patient underwent a right frontal craniotomy and resection of the brain tumor. During the surgery, the tumor adherent to the dura was evident. A gross total resection was obtained with removal of the area of thickened dura with margin.
Pathology
Pathology from the right frontal brain extra-axial mass resection, reviewed at the National Institutes of Health (NIH) and National Cancer Institute (NCI), revealed an intermediate-grade myxoid sarcoma, with a mitotic rate that was less than 10/10—making it unlikely that the tumor had metastasized. However, necrosis was present.
Postsurgical Diagnostics
A postoperative MRI of the brain showed no residual tumor. Lumbar puncture with cerebral spinal fluid (CSF) analysis showed rare monocytes and mature lymphocytes that were negative for acute inflammation or malignancy. A staging PET/CT scan showed postoperative changes in the right frontal lobe, with no metabolic evidence of residual disease. Enlarged hypermetabolic right parotid, right peri-parotid and right cervical nodes were evident, but presumed to be reactive from the surgery rather than indicative of metastatic disease.
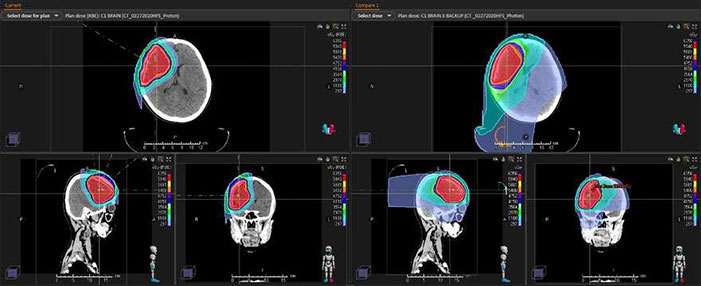
Postsurgical Treatment Plan
Postsurgical treatment options included chemotherapy and radiation therapy. Molecular testing was obtained to personalize systemic therapy. While the patient has a rare intermediate-grade intracranial sarcoma, focal radiotherapy is generally recommended postoperatively to improve local tumor control and decrease risk of disease recurrence. Proton beam radiotherapy was chosen to minimize long-term toxicity and complications from cranial radiation, and to more safely escalate radiation dose to greater than 54 Gy. Proton beam radiation also may reduce the risk of long-term neurocognitive dysfunction, memory impairment, secondary malignancy and pituitary dysfunction when compared to conventional X-ray or photon radiation.